Fewer spinal surgeries: Welcome relief for California workers compensation
 Ask any cross-country traveler which state has the most beautiful scenery, and California usually ranks at or near the top. Unfortunately, the Golden State also takes top honors in a less flattering contest – some of the highest workers’ compensation costs in the country.
Ask any cross-country traveler which state has the most beautiful scenery, and California usually ranks at or near the top. Unfortunately, the Golden State also takes top honors in a less flattering contest – some of the highest workers’ compensation costs in the country.
It’s long been an expensive, bloated, inefficient system, saddled with a unique and costly medical lien system and plagued by fraud, loopholes, and unnecessary medical treatment.
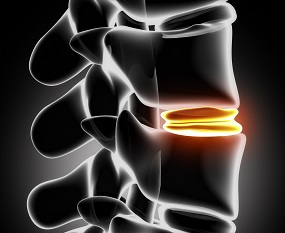
A case in point: spinal surgeries. For years, these costly procedures have been disproportionately performed in workers’ compensation cases compared to group health. Why? Financial incentives are one reason. Follow the money. A system of duplicate “pass-through” payments for hardware used in spinal surgeries has allowed hospitals to bill insurance carriers for the full cost of implants plus handling fees. It’s been the perfect incentive to perform unnecessary surgeries and implant unnecessary hardware.
Unfortunately for many patients, these unnecessary procedures have led to complications down the road. On top of that, a new study published in the journal Spine shows that outcomes for injured workers who undergo spinal surgeries aren’t significantly different from the outcomes for those treated non-surgically for back problems, so it’s clear many of these surgeries have been unnecessary.
Back to common sense for back injuries
Recent developments have started turning things around. The number of workers’ compensation hospitalizations for implant-eligible spinal surgeries dropped 21 percent from 2012 to 2014 according to a recent report by the California Workers’ Compensation Institute. It was the fourth year in a row those numbers declined.
What’s responsible for this sudden drop in spinal surgeries?
Our own president and CEO Byron Kerns says there are likely several factors:
- The phasing out of the duplicate “pass-through” payments
- The closing of loopholes in the workers’ compensation fee schedule
- SB863 reforms
Another likely contributing factor is the publicity that surrounded the scandal at Pacific Hospital in Long Beach, which averaged 585 implant-eligible spinal surgeries a year from 2008 to 2012. The hospital’s former owner pled guilty to paying kickbacks to doctors who referred patients for surgery.
With financial incentives for spinal surgeries drastically reduced, maybe doctors will start rethinking their decision to perform surgery as the automatic go-to solution for back injuries and take a more conservative approach.
Only the beginning
Although the reduction in workers’ compensation hospitalizations is good news, it doesn’t mean unnecessary surgeries are a thing of the past. Utilization reviews and independent medical reviews are still conducted without an actual exam of the patient, and there are still plenty of providers eager to recommend surgery.
These and other challenges continue to make it imperative for employers to have a proactive strategy for controlling workers’ compensation costs. At Republic Capital Claims Administrators, we’re committed to helping you do that. Contact us today, and if you haven’t already done so, download our free report, “How much could you save by self-insuring your work comp?”
